预后|【罂粟摘要】比较咪达唑仑、丙泊酚、右美托咪定镇静对急性心肌梗死危重患者预后的影响
比较咪达唑仑、丙泊酚、右美托咪定镇静对急性心肌梗死危重患者预后的影响
文章插图
贵州医科大学麻醉与心脏电生理课题组
翻译:任文鑫 编辑:陈锐 审校:曹莹
HOLIDAY
背景
关于急性心肌梗死(AMI)危重患者镇静治疗的研究较少。本研究旨在比较咪达唑仑、丙泊酚和右美托咪定对AMI危重患者预后的影响。
HOLIDAY
方法
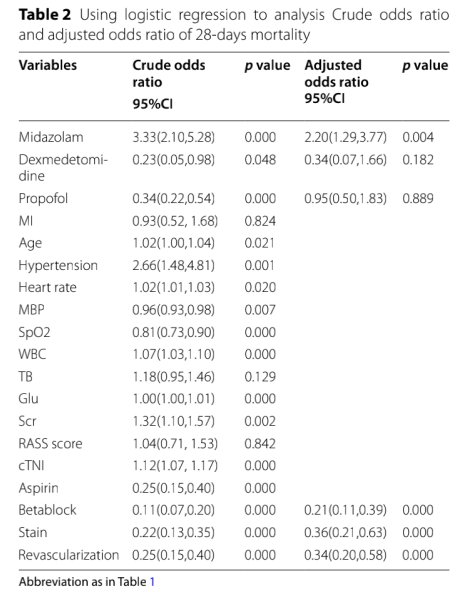
我们从重症监护III医疗信息集市(MIMIC III)数据库收集临床数据。427例使用镇静剂的AMI患者的数据来自冠心病重症监护病房(CCU)。从冠心病重症监护病房(CCU)采集了427名使用镇静剂的AMI患者的数据。
HOLIDAY结果
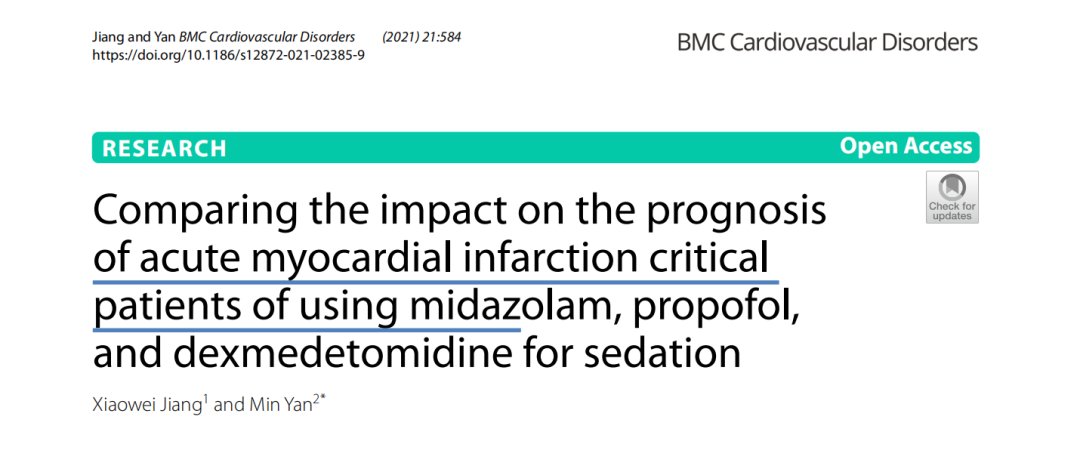
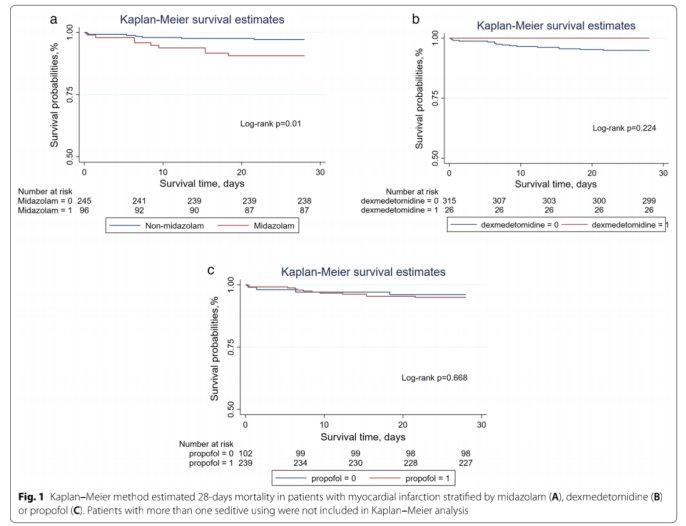
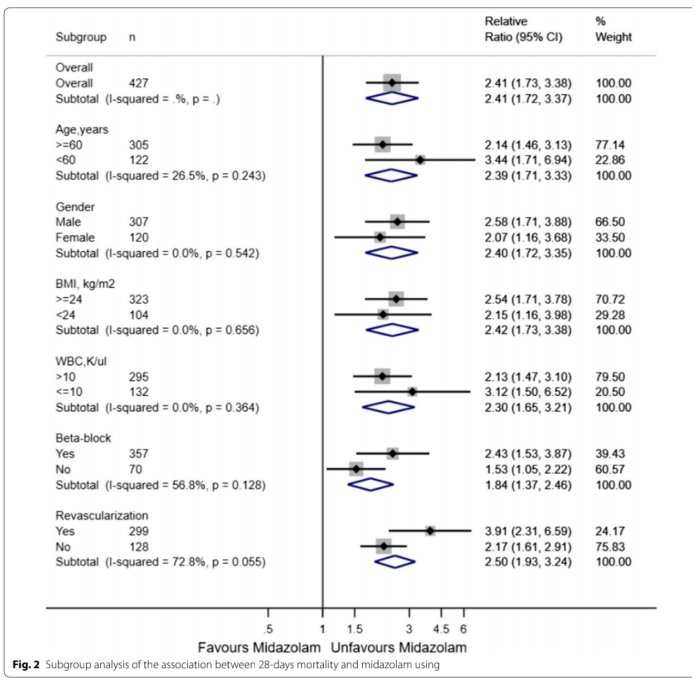
使用咪达唑仑患者有143例,使用丙泊酚患者有272例,使用右美托咪定患者有28例。总体患者28天死亡率为23.9%。通过逻辑回归分析结果表明,与使用丙泊酚或右美托咪定的患者相比,仅使用咪达唑仑的患者与增加28天死亡率显著相关。在年龄、性别、体重指数(BMI)、白细胞(WBC)、β受体阻滞剂和血运重建的亚组分析中,使用咪达唑仑与增加28天死亡率之间的相关性仍然显著。通过倾向评分匹配,140名使用咪达唑仑的患者和192名使用非咪达唑仑的患者成功匹配,使用咪达唑仑的患者CCU死亡率、住院死亡率和28天死亡率较高,机械通气时间和CCU持续时间较长。E值分析表明对未测量的混杂因素具有稳健性。
文章插图
文章插图
文章插图
文章插图
HOLIDAY结论
AMI危重患者首选丙泊酚或右美托咪定进行镇静治疗。
HOLIDAY 原始文献来源
Xiaowei Jiang,Min Yan.Comparing the impact on the prognosis
of acute myocardial infarction critical patients of using midazolam, propofol, and dexmedetomidine for sedation.Jiang and Yan BMC Cardiovascular Disorders (2021) 21:584.
Comparing the impact on the prognosis of acute myocardial infarction critical patients of using midazolam, propofol, and dexmedetomidine for sedation
Abstract
Background: There are less studies focusing on the sedative therapy of acute myocardial infarction (AMI) critical patients. This study aim to compare the impact on the prognosis of AMI critical patients of using midazolam, propofol and dexmedetomidine.
Methods: We collected clinical data from the Medical Information Mart for Intensive Care III (MIMIC III) database. Data on 427 AMI patients with sedatives using were recruited from in Coronary Heart Disease Intensive Care unit (CCU).
Results: There were 143 patients in midazolam using, 272 in propofol using and 28 in dexmedetomidine using. The rate of 28-days mortality was 23.9% in overall patients. Through logistic regression analysis, only midazolam using was signifcant association with increased 28-days mortality when compared with propofol or dexmedetomidine using. In the subgroup analysis of age, gender, body mass index (BMI), white blood cell (WBC), beta-block, and revascularization, the association between midazolam using and increased 28-days mortality remained signifcantly. Through propensity score matching, 140 patients using midazolam and 192 using non-midazolam were successfullymatched, the midazolam using presented with higher rate of CCU mortality, hospital mortality and 28-days mortality, longer of mechanical ventilation time and CCU duration. E-value analysis suggested robustness to unmeasured confounding.
【 预后|【罂粟摘要】比较咪达唑仑、丙泊酚、右美托咪定镇静对急性心肌梗死危重患者预后的影响
- 疫苗|【992 | 速看】传播能力有所增强!有关奥密克戎变异株,最新解答来了!
- 血压|主动脉夹层可夺命?这五类人是高危人群,需高度重视
- 肺炎|遵义120教你肺炎伴胸膜炎怎么办
- 公司|罗欣药业:子公司注射用美罗培南通过仿制药一致性评价
- 相关|【中国实用外科杂志】肥胖代谢病合并甲状腺癌外科治疗中国专家共识(2021版)
- 范可尼|为什么会长白头发?
- 常崇旺|【视频回放】脑瘫患者常用外科术式及适应症
- 深圳|广东新增本土确诊病例9例:深圳2例、珠海5例、中山1例、梅州1例
- 痛风也可吃火锅 但注意少吃肉食
- 领导|邵阳召开强化新冠肺炎定点救治医院管理工作视频会议